Various Types of Toenail Fungus

Toenail fungus manifests in several forms, each with distinct characteristics. Subungual onychomycosis is the most common type, occurring beneath the nail plate and leading to thickened, discolored, and brittle nails. White superficial onychomycosis affects the nail's surface, causing white, crumbly spots that can spread and cover the entire nail if untreated. Candida onychomycosis, caused by yeast, often targets nails already damaged or exposed to moisture. This type results in swelling, pain, and a yellow-brown discoloration. Proper diagnosis by a podiatrist is essential to determine the specific type of infection and appropriate treatment. Antifungal medications, whether topical or oral, are typically used to combat these infections, helping restore nail health and prevent further complications. If you have developed a toenail fungus, it is strongly suggested that you confer with a podiatrist who can effectively treat the type you have.
For more information about treatment, contact one of our podiatrists of The Sun Healthcare & Surgery Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our offices located in Antioch, Martinez, and Concord, CA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
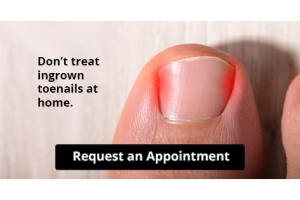
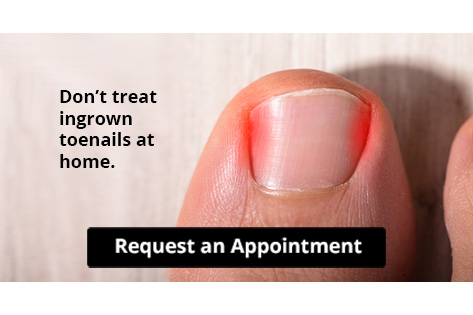
Let the Expert Treat Your Ingrown Toenails
Managing Pain of Diabetic Foot Problems
 Diabetic foot ulcers and peripheral neuropathy are common complications of diabetes, often resulting in significant pain and discomfort. Neuropathy, caused by prolonged high blood sugar levels, damages the nerves, leading to numbness, tingling, and pain in the feet. Ulcers develop due to reduced blood flow and the inability to sense injuries, allowing minor wounds to progress into serious infections. Assessment involves a thorough examination of the feet, checking for signs of neuropathy, poor circulation, and existing ulcers. Podiatrists use tools like monofilaments to test sensation and Doppler devices to assess blood flow. Management focuses on controlling blood sugar levels, proper wound care, and preventing further complications. Pain from neuropathy is treated with medications, while ulcers require cleaning, debridement, and specialized dressings. Custom orthotics and appropriate footwear can alleviate pressure on affected areas. If you suffer from diabetic-related foot problems, it is suggested that you are under the care of a podiatrist for optimal care.
Diabetic foot ulcers and peripheral neuropathy are common complications of diabetes, often resulting in significant pain and discomfort. Neuropathy, caused by prolonged high blood sugar levels, damages the nerves, leading to numbness, tingling, and pain in the feet. Ulcers develop due to reduced blood flow and the inability to sense injuries, allowing minor wounds to progress into serious infections. Assessment involves a thorough examination of the feet, checking for signs of neuropathy, poor circulation, and existing ulcers. Podiatrists use tools like monofilaments to test sensation and Doppler devices to assess blood flow. Management focuses on controlling blood sugar levels, proper wound care, and preventing further complications. Pain from neuropathy is treated with medications, while ulcers require cleaning, debridement, and specialized dressings. Custom orthotics and appropriate footwear can alleviate pressure on affected areas. If you suffer from diabetic-related foot problems, it is suggested that you are under the care of a podiatrist for optimal care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from The Sun Healthcare & Surgery Group. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Antioch, Martinez, and Concord, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Possible Causes of Heel Pain
 Heel pain can stem from various conditions. Plantar fasciitis, the inflammation of the thick band of tissue running along the bottom of the foot, often causes stabbing pain near the heel. Bursitis, an inflammation of the fluid-filled sacs cushioning the heel, can result from repetitive stress. Heel spurs, bony growths on the underside of the heel bone, may develop due to long-term strain on foot muscles and ligaments. A pump bump, or Haglund's deformity, is a bony enlargement on the back of the heel caused by pressure from footwear. Achilles tendonitis is inflammation of the Achilles tendon, typically due to overuse or tight calf muscles. Diagnosing heel pain involves having a physical exam, reviewing medical history, and sometimes undergoing imaging tests, such as X-rays or MRI scans. Treatment options include rest, stretching exercises, orthotics, and anti-inflammatory medications. If you have persistent heel pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment plan.
Heel pain can stem from various conditions. Plantar fasciitis, the inflammation of the thick band of tissue running along the bottom of the foot, often causes stabbing pain near the heel. Bursitis, an inflammation of the fluid-filled sacs cushioning the heel, can result from repetitive stress. Heel spurs, bony growths on the underside of the heel bone, may develop due to long-term strain on foot muscles and ligaments. A pump bump, or Haglund's deformity, is a bony enlargement on the back of the heel caused by pressure from footwear. Achilles tendonitis is inflammation of the Achilles tendon, typically due to overuse or tight calf muscles. Diagnosing heel pain involves having a physical exam, reviewing medical history, and sometimes undergoing imaging tests, such as X-rays or MRI scans. Treatment options include rest, stretching exercises, orthotics, and anti-inflammatory medications. If you have persistent heel pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment plan.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of The Sun Healthcare & Surgery Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Antioch, Martinez, and Concord, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
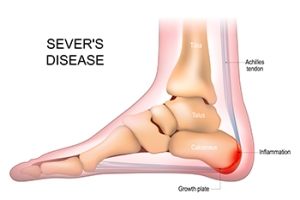
Sever's Disease and How to Find Relief
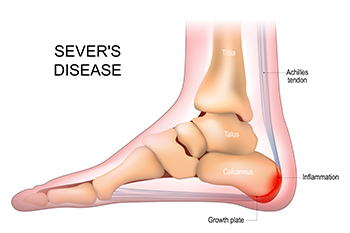
Sever's disease, also known as calcaneal apophysitis, is a common cause of heel pain in children and adolescents, particularly those who are active in sports. This condition occurs when the growth plate at the back of the heel becomes inflamed due to repetitive stress or tension. As children's bones grow faster than their muscles and tendons, excessive pulling on the heel's growth plate can lead to discomfort, swelling, and tenderness. Identifying Sever's disease typically involves a thorough examination by a podiatrist, including a review of symptoms and a physical assessment. While the condition often resolves on its own once growth plate closure occurs, there are several strategies for managing symptoms and finding relief. These may include rest, stretching exercises, and supportive footwear with cushioning insoles. If your active child has heel pain, it is suggested that you visit a podiatrist who can diagnose if it is Sever's disease, and offer the appropriate treatment method.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from The Sun Healthcare & Surgery Group. Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Antioch, Martinez, and Concord, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
How Flip-Flops Impact Feet

Flip-flops are a popular choice for casual footwear, especially as the weather warms up. However, their impact on foot health is a subject of ongoing debate. Typically, flip-flops offer minimal support to the arches of the feet, which can lead to problems such as plantar fasciitis or other forms of foot pain. The design of flip-flops forces the toes to grip the soles in order to keep the footwear in place while walking. This unnatural holding action can alter the way one walks, potentially causing long-term changes in foot structure and gait. The lack of cushioning and support also means that the feet are more vulnerable to injuries from stepping on sharp objects or from the stress of walking on hard surfaces. If you enjoy wearing flip-flops and are experiencing foot discomfort or changes in your walking pattern, it is suggested that you consult a podiatrist to determine the best footwear for your needs.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact one of our podiatrists from The Sun Healthcare & Surgery Group. Our doctors will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our offices located in Antioch, Martinez, and Concord, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.